
Applying action mapping to help clinicians build empathy and trust in digital consultations.

It started with an awkward conversation. A nurse tried to comfort a patient online, but the patient felt misunderstood and unseen. This moment – and others like it – inspired a project that we are deeply proud of. At its heart, this project was about understanding the people we design for – their needs, their struggles, and the moments that matter to them. Getting there required a rare mix of collaboration and vulnerability, the kind that doesn’t often emerge from subject matter experts (SMEs). So often, training projects launch with the best of intentions only to fall short because of a reluctance to have awkward conversations. The result? The learner’s needs are sacrificed on the altar of “training for training’s sake.” But every now and then, the stars align. The right questions are asked. The right stories are shared. The right people come to the table. This was one of those times.

One of our partners is a South African HealthTech company offering a centralised medical communications and medical history database, and online doctor services through pharmacy clinics. Its services bridge the gap between South Africa’s over-serviced private healthcare sector and its strained public sector by providing quality, affordable, and convenient care.
As a growing organisation, this HealthTech company is constantly hiring new medical staff. These new hires often come from years of working in public hospitals or clinics and suddenly find themselves in an online, private sector role. Their clinical expertise is strong. But the shift to digital practice exposes more nuanced gaps in soft skills like patient communication, empathy, and trust.
Imagine a nurse who has worked for years in a bustling public ward, now trying to build a personal, human connection online.
The challenge goes beyond technical proficiency. It’s about making a patient feel seen and heard through a screen.
This was the challenge the HealthTech company brought to us: train staff in soft skills. What those soft skills were, exactly, remained to be discovered. As with every project we do together, we started with a workshop.

To get to the heart of our learners’ needs, we drew inspiration from Cathy Moore’s brilliant book, “Map It: The Hands-on Guide to Strategic Training Design”. Its guiding premise is simple: begin by understanding the problem and why it’s happening. Then define the behaviours you want to see.
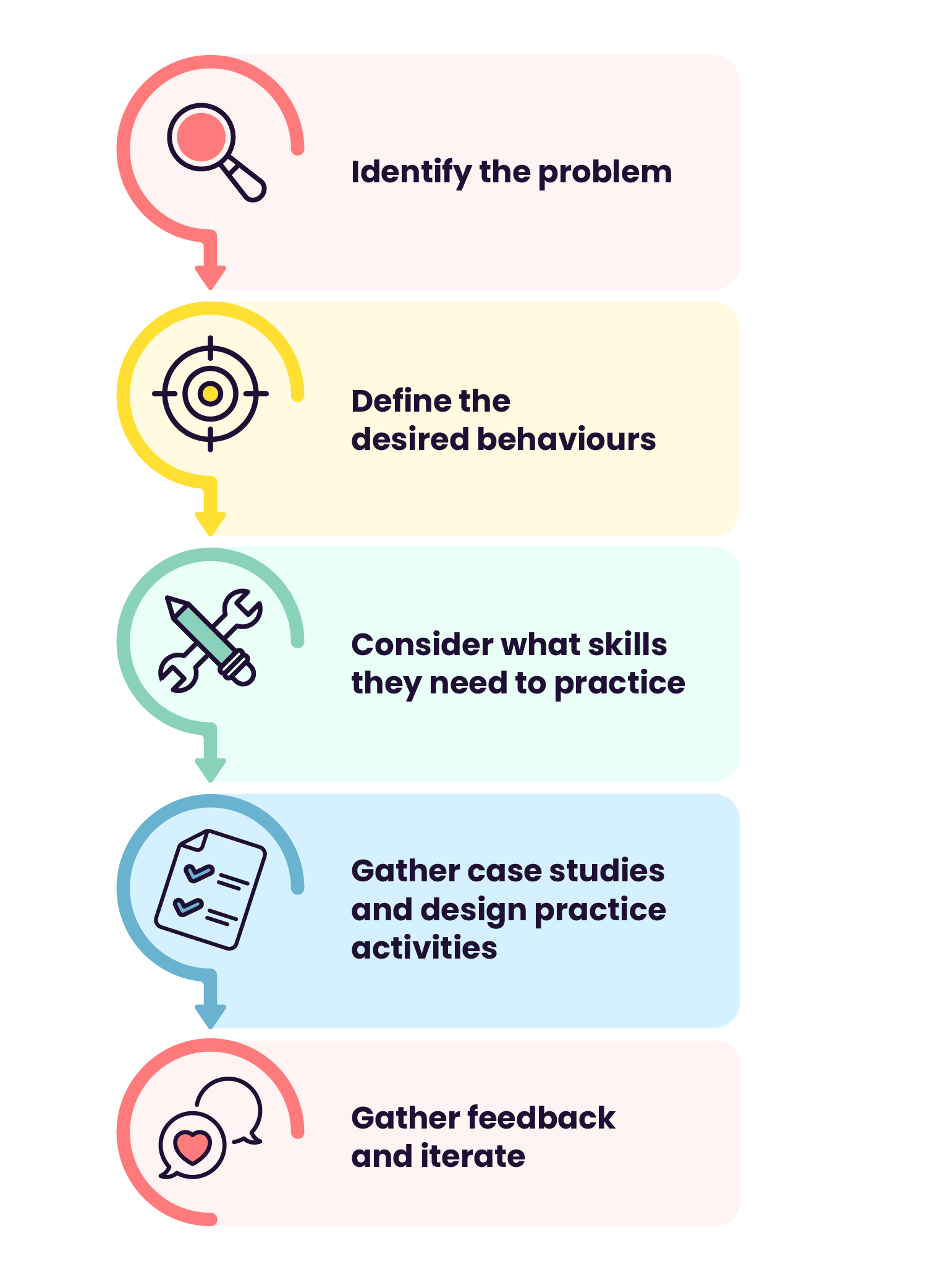
With that in mind, we brought together five medical staff from the HealthTech company for an online workshop. Ahead of time, we did some digging online and collected patient reviews from various sources. We challenged the SMEs to analyse, engage, and respond to these to discern which could be addressed by our training. Our goal was to pinpoint the problem, and that meant inviting honesty, reflection, and even discomfort.
We asked questions like:
The next hour and a half flew by. The stories weren’t about bad medical practice or careless staff. They were about moments that felt awkward, moments when words weren’t enough, moments when patients felt overlooked.
Through this collaborative conversation, a theme emerged: unmet patient expectations.
With this clarity, we created an online course to help clinicians engage more empathetically, build trust with patients, and develop a deeper awareness of patients’ experiences during consultations.

Here are two examples of how those deep conversations shaped our final training:
One early insight was how easily medical staff forget that medical language can alienate patients.
Think about it – many of us have left a doctor’s office thinking, “Wait, what just happened?” In online consultations, this problem can intensify. Patients may feel intimidated or misunderstood when medical terms dominate the conversation.
We assumed what we knew to be true: these staff care deeply about their patients.
The problem wasn’t a lack of empathy, but a lack of awareness.
So we built scenarios where learners could experience both sides of the conversation.
In one lesson, learners meet Nurse Liyanda. In focusing purely on medical details, she leaves the patient, Nkosazana, feeling unseen and unheard. As learners walk through the lesson from both the nurse’s and patient’s point of view, they gain a deeper understanding of how words can alienate or invite trust.
Another challenge surfaced: online consultations introduce a “digital divide” between patient and medical professional. Even tiny moments – a glance away, a distracted expression – can make a patient feel ignored.
To explore this, we introduced another character, a passionate nurse trying to balance patient care with the demands of a digital workspace. Through this lens, learners came to understand how subtle gestures can have a profound emotional impact. In an online consultation, focus and presence are as vital as clinical expertise.

So, was all this worth it? The results speak for themselves.
We measured the effectiveness of the training by comparing pre‑ and post‑course survey results.
In specific areas related to unmet patient expectations, learner confidence rose by 22.5%, 22.1%, and 36.4%.
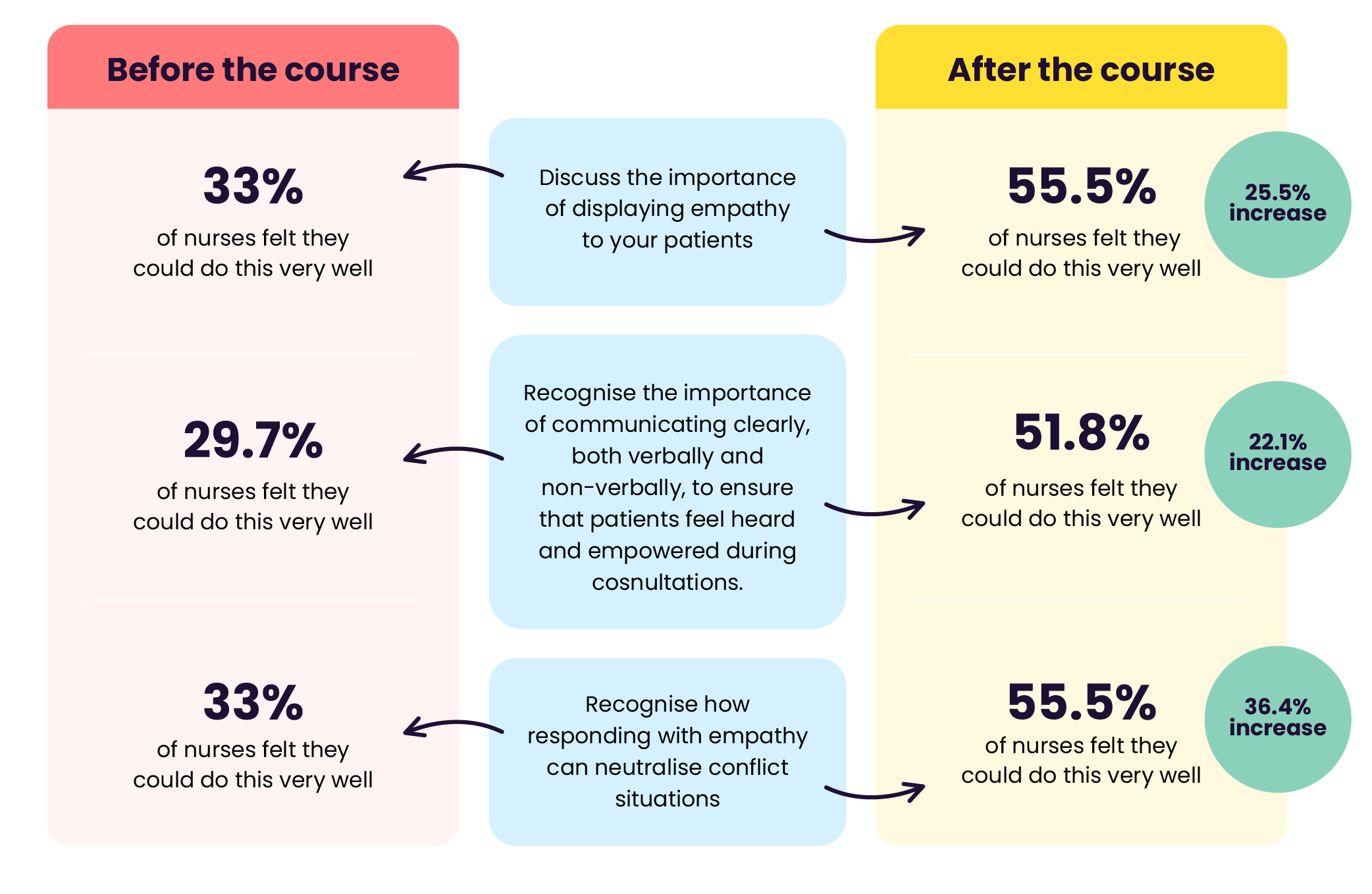
We also collected learner feedback through a comments section, which offered valuable insights into our learners' experiences, highlighting what they enjoy and the areas where we can improve. Learner comments about the effectiveness of the examples indicate that the content resonates with them and is relevant to their everyday lives.
Every aspect of this project was collaborative. Every step required stakeholders to slow down, ask hard questions, and listen deeply. The results reaffirmed what we’ve always believed: understanding the problem is the first step to creating a solution that truly works.
Behind every online consultation is a person hoping to be heard.
By embracing vulnerability and collaboration in the design process, we can help create training that doesn’t just teach – it transforms.
And in doing so, we help clinicians build trust, deepen connections, and ultimately deliver better patient care.
That, after all, is the point.
Want to design high-impact learning experiences with us? Get in touch at hello@whosyouraddie.com to discuss your project.
